Once You Repair Obliteration Can You Sell It?
- Enquiry article
- Open Access
- Published:
A neglected problem in the utilization of complimentary anterolateral thigh flap toward reconstructing complicated wounds of extremities: the obliteration of deep dead space
Journal of Orthopaedic Surgery and Research volume xv, Article number:483 (2020) Cite this article
Abstruse
Groundwork
Deep expressionless space may be thought as an independent risk factor of the poor infection control later on flap reconstruction in circuitous limb wounds. Only it tin can exist easily neglected. The conventional skin flap and musculocutaneous flap are difficult to obliterate the deep dead space in irregular shape effectively. It was investigated that the clinical awarding of chimeric anterolateral thigh perforator flap in the treatment of complex wounds complicated with deep dead space of the extremities in the paper.
Methods
50-six cases complicated with deep dead space wounds were registered in group. Post-obit thorough debridement and treatment with VSD, the granulation tissues grew with well-controlled infection. And then the chimeric anterolateral thigh perforator flap was used to obliterate the deep dead infinite and repair the wounds. The postoperative flap survival and infection weather were evaluated.
Results
Overall, the infection was effectively controlled, without persistent exudation or sinus tract germination subsequently wound healing. While 5 cases lost to follow-up, the remaining 51 cases were followed up until xv months on average. By and large, the affected extremities recovered satisfactorily with normal appearances and texture of the flaps, along with normal functions. Chiefly, no recurrence of infection was observed.
Determination
During the grafting of chimeric perforator flap pedicled with lateral thigh musculus flap, the muscle flap is recommended to obliterate the deep dead space while the skin flap is being used to cover the wound. The combination of these 2 technologies performed well in the repair and reconstruction of the complex wounds of the extremities, possessing potential for broader clinical application.
Groundwork
Microsurgery is an effective handling toward diverse types of wounds in the extremities caused by high-energy trauma in clinical settings. High clinical efficacy has been reported in a large number of studies. Amongst these studies, free flaps were recommended to be used in the treatment of extensive soft-tissue defects or complex wounds, while patients with poor surrounding soft tissue could not have the local pedicled flap. Since its first description past Vocal et al. [ane] in 1984, the anterolateral thigh flap has been considered to be an universal and preferential gratuitous flap [2, 3] for the reconstruction of limb wounds, owing to its abiding anatomical position of nutrient vessels, long vascular pedicle, thick vascular diameter, and relatively concealed donor site. Our group previously utilized the anterolateral thigh flap to reconstruct diverse types of wounds to achieve satisfactory outcomes [4, 5]. However, repeated exudation and persistent infection surrounding the postoperative flaps in partial complex wounds occurred during the handling process. Specially, local deep expressionless space was constantly observed during the 2nd debridement and a large quantity of inflammatory tissues was noted. Nosotros believe that these wounds complicated with deep dead space may be an independent risk factor of the poor infection control after flap reconstruction, and the management of deep dead infinite plays an of import function throughout the reconstruction of circuitous limb wounds.
Afterwards multiple times of debridement of deep tissue injuries, related to the mail service-traumatic ischemic necrosis and the limb infection, some patients experience wounds with balance deep dead space [6]. The three-dimensional characteristic of the residual deep expressionless infinite is associated with the poor claret supply, unsuccessful effusion drainage, and deficient granulation growth. These factors may provoke or aggravate the infection that requires further debridement. Also, the deep dead space may be enlarged after debridement, bringing challenges to the reconstruction in clinical settings in a brutal cycle design. To forbid this pattern, it is essential to obliterate the deep expressionless space with live tissues that cover the wound and improves blood supply, for the promotion of the growth and healing of the tissue around the cavity. According to previous reports, conventional flap transplantation tin can just cover the superficial wounds [v, seven, 8]. Despite the advantages such as splendid appearance and mild injury induction of the perforator, it fails to obliterate the deep dead space caused by trauma. Conventional musculocutaneous flap is formed by the musculocutaneous perforating branch from the vascular pedicle. The skin flap and muscle flap receive blood supply from the same perforating branch, thus making it difficult to separate them. The fractional sliding does not fulfill the requirements of flexibilities to effectively obliterate the deep dead space. Regarding biomaterials, bone cement and negative pressure sponge for vacuum sealing drainage (VSD) take been ordinarily applied equally temporary filling materials to obliterate the deep expressionless space [ix,x,11], due to the lack of biological activities. With the development of flap grafting technique, especially the broader adaption of chimeric perforator flap, other tissue flaps are incorporated when incising the skin flap. Specifically, the pare flap is responsible to embrace the wounds, while the other tissue flaps, such as muscle flap, are employed to obliterate the deep dead infinite [12]. To meliorate meet the clinical requirements, we used the chimeric anterolateral thigh perforator flap (chimeric perforator flap pedicled with descending branch of the lateral circumflex femoral avenue and lateral thigh muscle flap) to treat wounds complicated with deep dead infinite of the extremities with slight modification from previous reconstruction methods. In this study, clinical data of 56 cases admitted to our hospital from January 2022 to December 2022 were nerveless and retrospectively analyzed to evaluate the clinical efficacy of this modified technique.
Materials and methods
Inclusion and exclusion criteria
Inclusion criteria were as follows: all of these patients experienced severe extremity injuries accompanied by varying levels of tissue necrosis, tissue infection, and deep-tissue exposure. The residual deep dead space was observed after debridement. Information technology is suitable to utilise the anterolateral thigh flap to repair the wound. Exclusion criteria were as follows: patients unsuitable or unable to tolerate microsurgery.
Baseline data
50-6 cases were enrolled, aged 3-72 years with an boilerplate of 33.four years. The wound sized were from 8 cm × half dozen cm to 30 cm × 15 cm. Patient details are shown in Table one.
Treatment methods
Training prior to wound reconstruction
Co-ordinate to the conditions of the wound contamination or infection prior to wound reconstruction, 56 cases were treated with debridement and VSD as previously described [4, 5, 13]. Post-obit the wound cleaning, the chimeric perforator flap pedicled with descending branch of lateral circumflex femoral artery and lateral thigh muscle flap was applied to obliterate the deep dead space and reconstruct the wounds.
Operation process
General or combined spinal-epidural anesthesia was given. The patients were required to lay in a supine position. Preoperative Doppler ultrasound was performed to locate the descending branch of the lateral circumflex femoral artery. The microsurgical operations of 65 cases were performed past two different surgeons, all of whom had received systematic microsurgical preparation and had at least five years of contained microsurgical experience. Co-ordinate to the methods of Luo South et al. [14] and Lee YC et al. [fifteen], we designed the flap and exposed the perforating vessels of the flap. According to the size of deep expressionless space and the requirements of tissue reconstruction, one or more leaves of muscle flaps in an appropriate size and length were harvested with the descending branch of lateral circumflex femoral artery as the pedicle. The chimeric flap was grafted to the recipient site later on the incising of the pedicle. With the aligning of the distance between the chimeric flap and the vascular pedicle, the lateral thigh muscle flap was utilized to obliterate the deep expressionless space and the perforator flap was used to encompass the wound. The descending branch of the lateral circumflex femoral artery and its accompanying vein were anastomosed with the vessels at the recipient site under the microscope (Fig. 1). Specific adjustments were adopted according to the patient's conditions. For instance, nosotros enlarged the anastomosis sites of claret vessels by anastomosing the vessels of the skin flap with the distal vessels of the muscle flap for 5 cases with vascular separation betwixt the skin flap and muscle flap. In dissimilarity, the vascular pedicles of the lengthened flaps were grafted with the dandy saphenous vein or the descending co-operative of the lateral circumflex femoral avenue and vein [thirteen, 16], for half dozen cases with insufficient length of vascular pedicles.
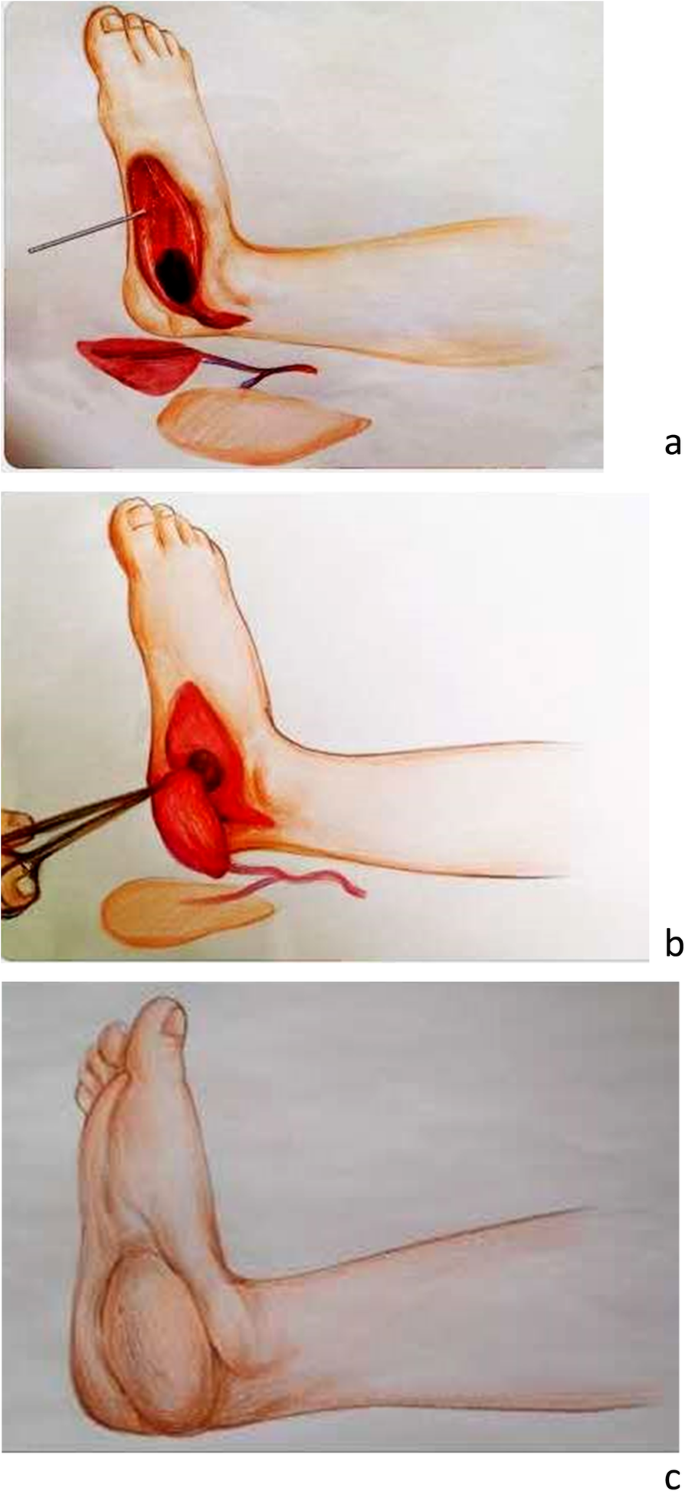
Diagram illustrated the blueprint procedure of chimeric anterolateral thigh perforator flap for the repair of circuitous wounds complicated with deep dead space of the extremity (a-c)
Postoperative management
Conventional microsurgical therapies, such as anti-inflammation, anti spasm, and anti-coagulation, were given every bit needed. According to preoperative bacterial civilization results, appropriate antibiotics were selected for subsequent treatment. The blood supply of the flap and the blood ooze below the flap were intensively monitored, and postoperative complications including vascular crises were timely and effectively managed. Based upon the status of wound and deep tissue reconstruction, active and passive rehabilitation exercises were actively carried out as soon as possible after the operation. Moreover, the survival and infection of flaps were evaluated postoperatively.
Results
Among 56 cases, 2 cases adult vascular crisis, which was alleviated with timely vascular exploration. One case had excessive haemorrhage subsequently flap grafting, which was resolved with surgical exploration. Three cases experienced partial necrosis of the flaps and, leaving remainder local wound, which were completely eliminated by secondary skin grafting in one instance and by proactive dressing changes in the other 2 cases. Overall, the infection was well controlled. No persistent exudation or sinus tract formation occurred later on wound healing. Except 5 cases lost to follow-upward, the remaining 51 cases were followed up until 15 months on average (ranged 9-24 months). Generally, the affected extremities recovered satisfactorily with normal appearances and texture of the flaps, along with normal functions. Importantly, no recurrence of infection was observed.
Typical cases were shown in Figs. 2, iii, and 4.

Case 1. A male patient, 49 years former, was admitted to our hospital due to postoperative deformity and infection of the correct foot for over six months. Upon access, a large quantity of purulent secretion was noted in the medial wounds of the right human foot, accompanied with sinus tract germination in the right calcaneus, stiffness, and deformity of the ankle (a). Later on admission, thorough debridement combined with VSD was performed (b). At one week after the VSD removal, granulation tissues surrounding the wounds grew well (c). The chimeric anterolateral thigh perforator flap was designed and harvested, and the perforator flap was thinned (d-f). The muscle flap was utilized to obliterate the dead space of calcaneal defects (one thousand, h). The skin flap was used for wound coverage and the blood supply was excellent after vascular anastomosis (i). During postoperative, twelve months follow-up, the foot infection was effectively controlled, with esthetic appearance of the skin flap (j, k), and the weight-bearing and walking functions of the pes was restored (l)
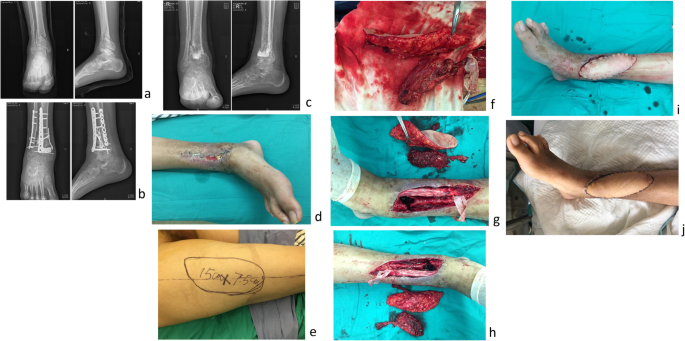
Case 2. A 24-year-old patient suffered from bilateral pilon fractures caused by loftier falling, open up fracture (Gustilo type II) on the right side. Afterward admission, thorough debridement was given, followed past internal fixation of the tibial and fibulal fractures (a, b), wound healing was poor, secondary infection occurred, and the internal fixation plate was exposed. The internal fixation plate was removed and filled with bone meal (c), but the wound infection remained uncontrolled (d). The chimeric anterolateral thigh perforator flap was designed and excised (due east, f). The muscle flap was employed to obliterate the dead infinite (g, h), the skin flap was used for wound coverage (i). Postoperative infection was well controlled and the flaps were normal in appearance and texture (j)

Case 3. A male person patient, 22 years former, was transferred from a local hospital due to postoperative infection for 2 weeks caused past traffic injury of the correct leg. Upon admission, extensive necrosis of the lateral soft tissues of the middle and lower right leg observed, accompanied with fracture of the centre fibula, free and exposed bones, and purulent secretions in the wounds (a, b). Upon admission, thorough debridement combined with VSD (twice) was performed, and granulation tissues surrounding the wounds grew well (c-e). The chimeric anterolateral thigh perforator flap was designed and harvested (f, g). The muscle flap was utilized to obliterate the dead infinite of the lateral leg, and the peel flap was used to cover the wound. The blood supply was excellent subsequently vascular anastomosis (h, i). The flap was normal in advent (j, thou). During postoperative follow-up for 12 months, no obvious sinus tract formation was observed and the infection was properly controlled
Word
Soft-tissue defects of extremities complicated with deep dead infinite caused by high energy injury bring challenges to the wound reconstruction in the clinical setting. Tissue defects, with poor local claret circulation, along with unsuccessful drainage often induce infections. In addition, some vital tissues and organs, such every bit bones, large blood vessels, nerves, muscles, tendons at a special site may be in the deep expressionless space. Therefore, we are facing a dilemma, since thorough debridement could lead to serious functional loss of these tissues or organs, whereas incomplete debridement could cause infections. Furthermore, some special deep dead spaces, which are associated with the articular cavity, internal fixation, pressure ulcer, or diabetes mellitus, farther increase the difficulty of wound reconstruction. The conventional peel flap and musculocutaneous flap are hard to obliterate the deep dead infinite in irregular shape finer. To overcome the challenges in these types of reconstructions associated with the three-dimensional requirement of the flap, the elimination of the deep dead space, besides equally the coverage of the very large soft-tissue defect in a single procedure with primary closure of the donor site are needed [17].
The chimeric perforator flap is a special form of perforator flap, which refers to two or more different types of independent tissue flaps (such as skin, fascia, muscle, and os) harvested in the aforementioned vascular supply expanse. At least 1 perforator flap is included in these independent tissue flaps, and the nutrient vessels originate from the same master claret vessels. Anastomosing a grouping of vascular pedicle (master blood vessels) can reconstruct the blood apportionment of multiple contained tissue flaps at the same time [17, eighteen]. In this study, we used the chimeric perforator flap pedicled with descending branch of lateral circumflex femoral artery, which is a special type of perforator flap [19]. In improver to the merits of traditional anterolateral thigh flap, information technology holds advantages as described in the post-obit. The claret supply of the multiple independent tissue flaps tin can be simultaneously reconstructed by anastomosing 1 group of claret vessels. This technique retains the advantages of musculocutaneous flap, such as excellent blood supply and potent anti-infection adequacy. Both perforator flap and muscle flap have vascular pedicles with a sufficient length. The lateral thigh muscle flap has excellent shaping ability, to finer obliterate irregular deep dead infinite. Moreover, the delivery of pare grafting on the exposed muscle flap minimizes the incisional expanse of peel flap, which is consequent with the concept of "advisable incision amount" without incising other ineffective tissues while incising the multi-leaf skin flaps and muscle flaps.
Thigh anterolateral muscle is rich, even if the amount of the harvested tissue is larger, besides will not cause limb dysfunction. In a study that involves 65 cases that underwent gratuitous anterolateral thigh chimeric flap reconstruction of defects in the caput and neck regions, Kun Wu et al. [2] reported a new classification concept to divide the anterolateral thigh chimeric perforator flap into three types: trunk blazon (I type, xvi.9%), branch blazon (Two type, 69.iii%), and bifurcation type (3 type, 13.viii%). It had certain significance for all kinds of tissue defect repair. In our present written report, 5 cases showed vascular variations, in which the skin flap and muscle flap vessels were separated and did non originate from the common junction. To solve this trouble, a novel chimeric flap was developed by anastomosing the nutrient vessels of the perforator flaps with the distal vessels of the muscle flaps.
The chimeric perforator flap pedicled with descending branch of lateral circumflex femoral artery is a novel and applied procedure, which achieves 3-dimensional reconstruction of the wounds with an expanded application range of flaps for the reconstruction of complex soft-tissue defects of the extremities. There are some previous studies that utilized similar concept but different details. For example, N.A.S. Posch et al. [xx] used combined free partial vastus lateralis with anterolateral thigh perforator flap to reconstruct extensive composite defects. Qing 50 et al. [21] designed private vastus lateralis musculus-chimeric multi-lobed anterolateral thigh perforator flap to reconstruct circuitous three-dimensional defects in the extremities. Zheng Ten, et al. [22] performed single-phase reconstruction and revascularization using a free flow-through chimeric anterolateral thigh perforator flap under emergency.
We reconstruct the limb defects complicated with residual deep dead space in 56 cases and accomplished high clinical efficacy in 51 cases with complete post-operational follow-up, while no persistent wound exudation or sinus tract formation observed. Consistently, in the report of adult chronic tibial osteomyelitis cases, Buono P et al. [23] demonstrated that fasciocutaneous and perforator free flaps offer a comparable efficacy to the muscle flaps for infection treatment, with a significantly higher patient satisfaction and esthetic result. To be noted, the cases of extremity defects complicated with the closure of deep expressionless space were included in our current study, and alternative surgical methods should exist combined for those with structural tissue defects. If structural tendon, nervus, and bone tissue defects were observed at the recipient site, the reconstruction of these tissues should be performed using techniques such as free revascularized fibula and iliac crest bone flaps [24] or Ilizarov technique [25], and Mesquelet technique [26]. Postoperative clinical efficacy and limb function of these methods were not to be described here.
In this study, the vascular crisis occurred in ii cases after operation and extensive haemorrhage occurred in ane case after flap grafting, which requires accurate judgment and precise functioning to exist dealt with. The main crusade of vascular crisis is thrombosis [27], associated with the quality of blood vessels at the recipient site, such as the intimal separation, especially in patients with serious contusion, long-term wound infections, diabetes mellitus, smoking, onetime historic period, etc. Consequently, it is essential to dissect and separate the healthy vessels to anastomose with the vessels at the donor site. Because the perforating branch vessels are relatively sparse, a certain amount of surrounding tissues should be preserved to avoid baloney, traction, or compression of the perforating branch vessels. Peculiarly, vascular traction could be acquired by extensibility of musculus during the filling of a muscle flap. Moreover, attention should be paid to hemostasis at the recipient wounds, the incised peel flap, and muscle flap, especially for the inflammatory granulation tissues with sufficient claret supply. If intraoperative hemostasis were not performed effectively, the anticoagulant and anticonvulsant drugs were used after operation, and pressure bandage could not be practical to the wound in the recipient area, then massive hemorrhage or hematocele at the wound sites would occur.
Conclusions
Deep dead space is a problem in the procedure of limb wound reconstruction that can be easily neglected. The chimeric perforator flap pedicled with a descending branch of lateral circumflex femoral artery can be applied to treat limb wounds complicated with remainder deep dead infinite, which uses muscle flap to effectively obliterate the deep dead space and employs perforator flap to cover the wounds. This technique in our study yields satisfactory clinical efficacy, providing foundations for further clinical application.
Availability of data and materials
None
References
-
Song YG, Chen GZ, Vocal YL. The free thigh flap: a new free flap concept based on the septocutaneous avenue. Br J Plast Surg. 1984;37:149–59.
-
Wu Thou, Ji T, Cao West, Wu HJ, Ren ZH. Application of a new nomenclature of chimeric anterolateral thigh free flaps. J Craniomaxillofac Surgery. 2022;47:1198–202.
-
Zhang Y, Gazyakan E, Bigdeli AK, Will-Marks P, Kneser U, Hirche C. Soft tissue gratuitous flap for reconstruction of upper extremities: a meta-analysis on event and safety. Microsurgery. 2022;39:463–75.
-
Li RG, Ren GH, Tan XJ, Yu B, Hu JJ. Complimentary flap transplantation combined with peel grafting and vacuum sealing drainage for repair of circumferential or sub-circumferential soft-tissue wounds of the lower leg. Med Sci Monit. 2022;xix:510–vii.
-
Li RG, Yu B, Wang Thousand, Chen B, Qin CH, Guo K, et al. Sequential therapy of vacuum sealing drainage and gratis-flap transplantation for children with extensive soft-tissue defects below the human knee in the extremities. Injury. 2022;43:822–8.
-
Franke A, Hentsch S, Bieler D, Schilling T, Weber Due west, Johann M, et al. Direction of soft-tissue and bone defects in a local population: plastic and reconstructive surgery in a deployed armed services setting. Mil Med. 2022;182:e2010–twenty.
-
Zheng X, Zheng C, Wang B, Qiu Y, Zhang Z, Li H, et al. Reconstruction of complex soft-tissue defects in the extremities with chimeric anterolateral thigh perforator flap. Int J Surg. 2022;26:25–31.
-
Spyropoulou A, Jeng SF. Microsurgical coverage reconstruction in upper and lower extremities. Semin Plast Surg. 2022;24:34–42.
-
Huang HJ, Niu XH, Yang GL, Wang LY, Shi FC, Xu SJ, et al. Clinical furnishings of application of antibiotic bone cement in wounds of diabetic foot ulcers. Zhonghua shao shang za zhi=Zhonghua shaoshang zazhi = . Mentum J Burns. 2022;35:464–half dozen.
-
Cuff MJ, Yoon RS, Egol KA, Liporace FA. Uses of negative force per unit area wound therapy in orthopedic trauma. Orthop Clin Due north Am. 2022;46:227–34.
-
Liu 10, Liang J, Zao J, Quan L, Jia 10, Li M, et al. Vacuum sealing drainage treatment combined with antibiotic-impregnated bone cement for treatment of soft tissue defects and infection. Med Sci Monit. 2022;22:1959–65.
-
Numajiri T, Fau SY, Nishino K, Fau NK, Sugimoto K, Fau SK, Iwashina Y, Fau IY, Ikebuchi Chiliad, Fau IK, Nakano H, et al. Successful retrograde arterial inflow through a muscular co-operative in a free anterolateral thigh chimeric flap transfer. Microsurgery. 2022;34:four.
-
Gao-Hong R, Run-Guang L, Gui-Yong J, Chao-Jie C, Zhi-Gang B. A solution to the vessel shortage during free vascularized fibular grafting for reconstructing infected bone defects of the femur: Bridging with vein transplantation. Injury. 2022;48:486–94.
-
Luo S, Raffoul Due west, Luo J, Luo Fifty, Gao J, Chen L, et al. Anterolateral thigh flap: a review of 168 cases. Microsurgery. 1999;19:232–8.
-
Lee YC, Chen WC, Chou TM, Shieh SJ. Anatomical variability of the anterolateral thigh flap perforators: vascular anatomy and its clinical implications. Plast Reconstr Surg. 2022;135:1097–107.
-
Echo A, Bullocks JM. Use of the descending co-operative of the lateral femoral circumflex vessels as a composite interposition graft in lower extremity reconstruction. Microsurgery. 2022;31:241–v.
-
Qing Fifty, Wu P, Yu F, Zhou Z, Tang J. Apply of a sequential chimeric perforator flap for i-stage reconstruction of complex soft tissue defects of the extremities. Microsurgery. 2022;40:167–74.
-
Hallock GG. The consummate classification for combined perforator flaps. Plast Reconstr Surg. 2022;127:1720–ix.
-
Cherubino G, Turri-Zanoni M, Battaglia P, Giudice Yard, Pellegatta I, Tamborini F, et al. Chimeric anterolateral thigh complimentary flap for reconstruction of circuitous cranio-orbito-facial defects after skull base cancers resection. J Craniomaxillofac Surg. 2022;45:87–92.
-
Posch NA, Mureau MA, Flood SJ, Hofer SO. The combined free fractional vastus lateralis with anterolateral thigh perforator flap reconstruction of extensive composite defects. Br J Plast Surg. 2005;58:1095–103.
-
Qing L, Wu P, Zhou Z, Yu F, Tang J. Customized reconstruction of complex iii-dimensional defects in the extremities with private design of vastus lateralis muscle-chimeric multi-lobed anterolateral thigh perforator flap. J Plast Surg Manus Surg. 2022;53:271–8.
-
Zheng X, Zhan Y, Li H, Zhang Z, Xue 10, Wang B, et al. Emergency repair of severe limb injuries with complimentary flow-through chimeric anterolateral thigh perforator flap. Ann Plast Surg. 2022;83:670–5.
-
Buono P, Castus P, Dubois-Ferriere V, Ruegg EM, Uckay I, Assal M, et al. Muscular versus non-muscular free flaps forsoft tissue coverage of chronic tibial osteomyelitis. World periodical of plastic surgery 2022;vii:294-300.
-
Mohlhenrich SC, Kniha K, Elvers D, Ayoub Northward, Goloborodko E, Holzle F, et al. Intraosseous stability of dental implants in free revascularized fibula and iliac crest os flaps. J Craniomaxillofac Surgery. 2022;44:1935–9.
-
Li R, Zhu One thousand, Chen C, Chen Y, Ren G. Bone transport for handling of traumatic composite tibial bone and soft tissue defects: any specific needs besides the Ilizarov technique? BioMed Res Int. 2022;2020:2716547.
-
Morelli I, Drago Fifty, George DA, Gallazzi Due east, Scarponi S, Romano CL. Masquelet technique: myth or reality? A systematic review and meta-analysis. Injury. 2022;47(Suppl six):S68–76.
-
Lee CH, Han SK, Dhong ES, Kim HP, Kim WK. The fate of microanastomosed digital arteries later on successful replantation. Plast Reconstr Surg. 2005;116:805–10.
Acknowledgements
We do not have acknowledgements..
Funding
Key Projects of President Foundation of Nanfang Hospital, Southern Medical University (2017A001); Shanghai Wang Zhengguo Trauma Medical Development Foundation (2017KJB-GK-001); Natural Scientific discipline Foundation of Guangdong Province (Approval no. 2022A030313640, 2022A1515012176); National Natural Science Foundation of China (81101366).
Author information
Affiliations
Contributions
Consummate the patient's treatment procedure: Gao-hong Ren, Da-yong Xiang, Xiao-hu Wu, Yun-biao Chen, and Runguang Li. Follow-up and data collection to patient: Xiao-hu Wu and Yun-biao Chen. Written report design: Gao-hong Ren and Runguang Li. Manuscript grooming: Gao-hong Ren and Runguang Li. Statistical analysis: Da-yong Xiang, Xiao-hu Wu, and Yun-biao Chen. All authors read and approved the terminal manuscript.
Respective author
Ethics declarations
Ideals blessing and consent to participate
The protocol was approved by the ideals committee of Southen Medical Academy. All patients agreed to participate in this paper and were consented accordingly.
Consent for publication
We agree to have this work publicized if accepted.
Competing interests
The authors do not have whatsoever competing interests.
Boosted information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Admission This article is licensed under a Creative Commons Attribution 4.0 International License, which permits utilize, sharing, adaptation, distribution and reproduction in any medium or format, as long as you requite appropriate credit to the original author(southward) and the source, provide a link to the Creative Commons licence, and signal if changes were made. The images or other tertiary political party material in this commodity are included in the commodity's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the commodity'southward Artistic Commons licence and your intended apply is not permitted by statutory regulation or exceeds the permitted utilize, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/iv.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/cypher/1.0/) applies to the data fabricated available in this article, unless otherwise stated in a credit line to the data.
Reprints and Permissions
About this article
Cite this article
Ren, Gh., Xiang, Dy., Wu, Xh. et al. A neglected trouble in the utilization of costless anterolateral thigh flap toward reconstructing complicated wounds of extremities: the obliteration of deep dead infinite. J Orthop Surg Res 15, 483 (2020). https://doi.org/x.1186/s13018-020-01914-0
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/ten.1186/s13018-020-01914-0
Keywords
- Chimeric flap
- Anterolateral thigh perforator flap
- Complex wounds
- Wound reconstruction
- Deep dead space
Source: https://josr-online.biomedcentral.com/articles/10.1186/s13018-020-01914-0
Posted by: mercedesspreduche.blogspot.com


0 Response to "Once You Repair Obliteration Can You Sell It?"
Post a Comment